Have you ever experienced a sudden, sharp pain in your lower back that made it difficult to even stand up straight? Perhaps you’ve felt a tingling sensation down your leg, or even a loss of strength in your foot? These could be signs of a broad-based disc bulge, a common condition that affects millions of people worldwide. While it can be a source of significant discomfort, understanding the underlying mechanisms and available treatment options can help you manage this condition effectively.
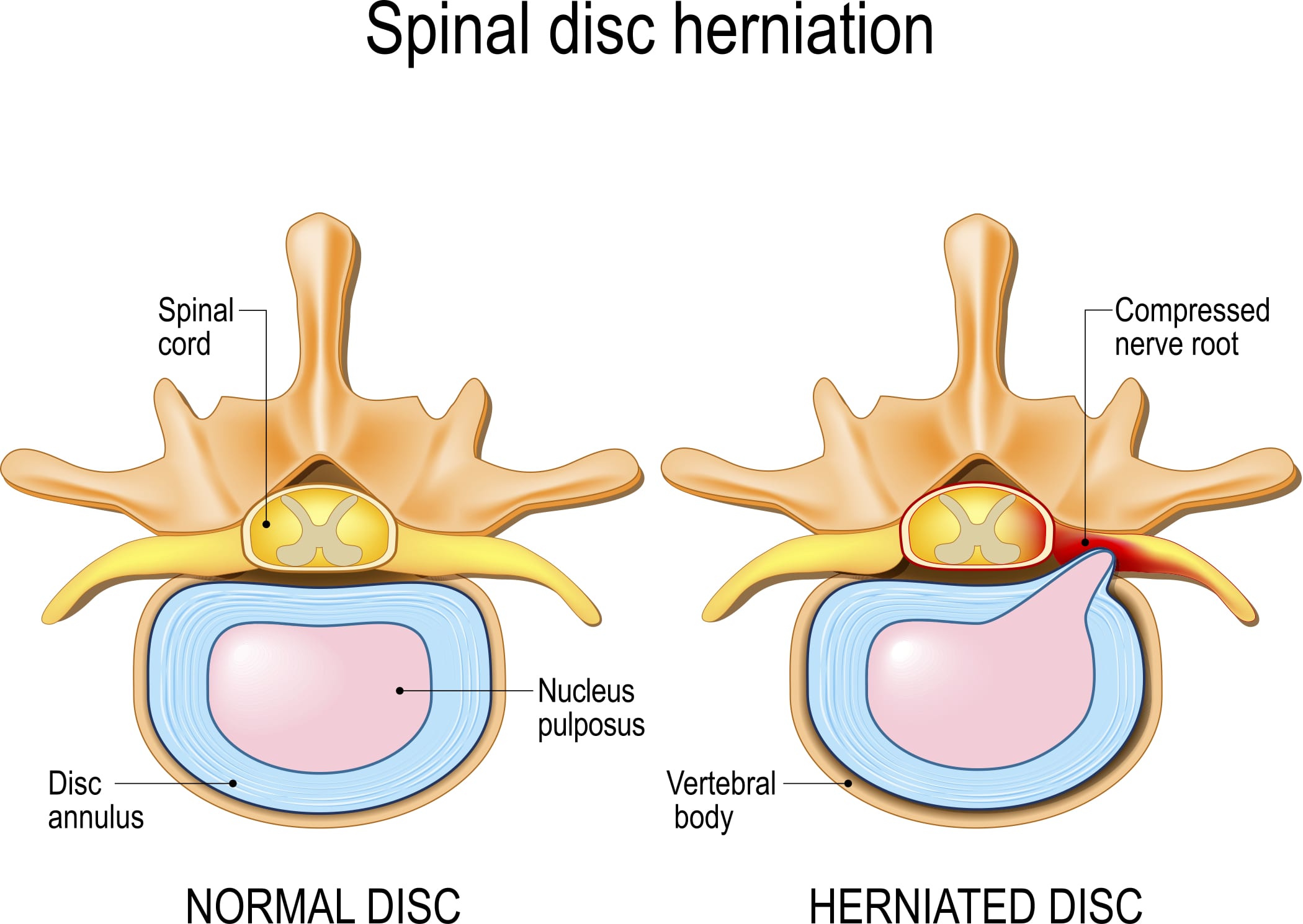
Image: upswinghealth.com
A broad-based disc bulge refers to a condition where the soft, gel-like center of an intervertebral disc protrudes beyond its normal boundaries, pushing against the surrounding nerves and affecting nearby structures. This bulge can occur in any part of the spine, but it is most common in the lumbar spine (lower back) due to the weight-bearing pressure and bending motions this region experiences. Understanding the anatomy of the spine and the role of intervertebral discs is crucial for comprehending the nature of a broad-based disc bulge.
Anatomy of the Spine: The Backbone of Our Body
Our spine, the central pillar of our body, is composed of 33 individual bones called vertebrae. These vertebrae are stacked upon each other, forming a flexible column that supports our head and trunk, allows movement, and protects the delicate spinal cord. Between each vertebra lies an intervertebral disc, a cushion-like structure that serves as a shock absorber and allows for the flexibility of the spine.
The Intervertebral Disc: A Shock Absorber and More
Each intervertebral disc is composed of two primary components: the annulus fibrosus, a tough outer ring made of fibrous cartilage, and the nucleus pulposus, a gelatinous core that acts as a shock absorber. The annulus fibrosus functions like a strong, flexible container for the nucleus pulposus, preventing it from bulging out. However, as we age or endure repetitive stress, the annulus fibrosus can weaken, making it more susceptible to tears and ruptures.
The Role of Discs in Movement and Stability
The intervertebral discs play a crucial role in allowing the spinal column to bend and twist while also providing stability. When the nucleus pulposus is healthy, it can distribute pressure evenly throughout the disc, ensuring smooth joint movement. However, when the annulus fibrosus weakens, the nucleus pulposus can start to push outward, creating a bulge that can press against surrounding nerves and structures.
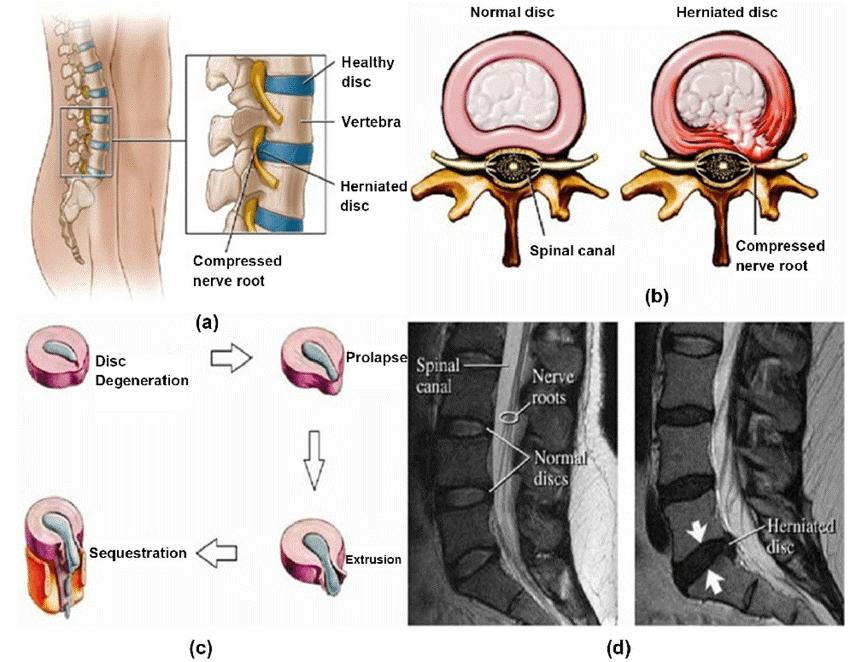
Image: gricechiro.com
What Causes a Broad-Based Disc Bulge?
A broad-based disc bulge is often a result of a gradual degeneration process that occurs over time. While age is a significant factor, other contributing factors can exacerbate the condition:
- Overuse and Repetitive Strain: Jobs or activities that involve repetitive lifting, bending, or twisting can put undue stress on the intervertebral discs, leading to gradual wear and tear.
- Poor Posture: Maintaining a position that puts continuous pressure on the spine, such as slouching or sitting for long periods without proper ergonomic support, can contribute to disc problems.
- Obesity: Excess weight adds stress to the spine, potentially increasing the pressure on the intervertebral discs and leading to bulging.
- Genetics: Some individuals are predisposed to developing disc problems due to familial history or genetic factors that affect the strength and integrity of their intervertebral discs.
- Trauma: A sudden impact to the spine, such as a slip, fall, or car accident, can cause tears in the annulus fibrosus and lead to a disc bulge.
The Gradual Deterioration of the Disk
The deterioration of an intervertebral disc is a gradual process that can start subtly and worsen over time. As the annulus fibrosus weakens, microscopic tears and fissures can develop, allowing the nucleus pulposus to seep out and create a bulge. This bulge can press against the surrounding nerves, leading to symptoms like pain, numbness, and tingling.
Symptoms of a Broad-Based Disc Bulge: Recognizing the Warning Signs
The symptoms of a broad-based disc bulge can vary widely depending on the location and severity of the bulge, as well as individual factors like age, fitness level, and overall health. However, some common symptoms include:
Back Pain: A Common Indicator
Back pain is the most prevalent symptom of a broad-based disc bulge. The pain can be sharp and stabbing, dull and aching, or even feel like a burning sensation. It may be localized to a specific area of the back or radiate to other parts of the body, such as the buttocks, legs, or feet. The intensity of the pain can range from mild discomfort to debilitating agony, often aggravated by certain movements or positions.
Sciatica: Pain Down the Leg
Sciatica, a pain that radiates down the leg, is a common symptom of a broad-based disc bulge in the lumbar spine. The pain can travel along the sciatic nerve, which runs down the back of the leg, and may be accompanied by numbness, tingling, or weakness in the foot or toes.
Numbness and Tingling: Sensory Alterations
Numbness and tingling can occur in the legs, feet, or even the buttocks as the bulging disc compresses the nerves. This sensory disturbance can be temporary or persistent, depending on the severity of the disc bulge.
Weakness: Loss of Muscle Strength
Weakness in the legs or feet can also be a symptom of a broad-based disc bulge, particularly if the bulge is compressing the nerve roots that control muscle function. This weakness can manifest as difficulty walking, lifting objects, or performing certain movements.
Diagnosis: Unraveling the Causes of Back Pain
Diagnosing a broad-based disc bulge involves a combination of medical history, physical examination, and imaging tests.
Medical History: Understanding the Patient’s Past
The doctor will ask about your medical history, including any previous injuries, surgeries, or medical conditions that might be relevant to your back pain. They will also inquire about your symptoms, their onset, duration, and severity, as well as any factors that seem to worsen or relieve your pain.
Physical Examination: Assessing Range of Motion and Neurological Function
A thorough physical examination is crucial for assessing your range of motion, muscle strength, and neurological function. The doctor will assess your back’s flexibility, identify painful areas, and test your reflexes and sensation in your legs and feet to determine the potential involvement of nerve compression.
Imaging Tests: Visualizing the Problem
Imaging tests play a vital role in confirming the diagnosis and determining the severity of the disc bulge. Commonly employed imaging techniques include:
- X-rays: These can reveal bone abnormalities and show the alignment of the spine, but they are not always sufficient to visualize the discs themselves.
- MRI (Magnetic Resonance Imaging): An MRI scan is the gold standard for visualizing soft tissues, including intervertebral discs. It can clearly show the extent of the disc bulge, any nerve compression, and surrounding structures.
- CT (Computed Tomography) Scan: A CT scan uses X-rays to create cross-sectional images of the spine. It can be useful in evaluating the alignment of the spine, identifying bone spurs, and providing additional details about the disc bulge.
Treatment: A Multifaceted Approach to Managing Broad-Based Disc Bulge
The treatment for a broad-based disc bulge aims to alleviate pain, reduce inflammation, improve mobility, and promote healing. The goal is to manage symptoms and prevent further deterioration of the disc. The treatment approach may vary depending on the severity of the disc bulge, the symptoms you experience, and your individual needs and preferences.
Non-Surgical Treatment: Conservative Approaches to Management
Most cases of broad-based disc bulge can be effectively managed with non-surgical treatments. These approaches focus on pain relief, reducing inflammation, and restoring mobility. Some common non-surgical treatment options include:
- Medications: Pain relievers, anti-inflammatories, and muscle relaxants can help manage pain and inflammation. In some cases, your doctor may prescribe corticosteroids, which can be injected into the area surrounding the affected disc to reduce inflammation directly.
- Physical Therapy: Physical therapy plays a crucial role in restoring mobility, strengthening muscles, improving posture, and teaching proper body mechanics to prevent further injury. Exercises specifically designed to improve core strength, flexibility, and balance can help stabilize the spine and reduce pain.
- Rest and Activity Modification: Resting the affected area can help reduce pain and inflammation. However, prolonged bed rest is not recommended as it can lead to muscle weakness and stiffness. Your doctor or physical therapist may recommend specific activities to help you gradually regain your strength and mobility while taking precautions to avoid exacerbating your symptoms.
- Heat and Cold Therapy: Applying heat can help relax muscles and soothe pain, while applying cold can reduce inflammation. These therapies can be used alternately to help manage symptoms.
- Over-the-Counter Pain Relief: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce pain and inflammation. However, it is essential to consult your doctor before starting any new medication.
- Bracing: In some cases, a back brace may be recommended to provide support and reduce strain on the affected disc.
Surgical Intervention: When Non-Surgical Treatments Fail
Surgical intervention is generally reserved for severe cases of broad-based disc bulge where conservative treatments have failed to provide relief or where the bulge is significantly compressing nerves, leading to significant neurological deficits. Surgical options may include:
- Discectomy: This is a surgical procedure to remove the bulging or herniated part of the disc, relieving pressure on the nerves. A discectomy can be performed through an open incision or laparoscopically, a minimally invasive technique that involves smaller incisions.
- Spinal Fusion: In some cases, spinal fusion may be recommended if the disc bulge has caused instability in the spine. This procedure involves joining two or more vertebrae together, eliminating the movement between them and providing stability. Spinal fusion can involve bone grafts or synthetic materials to promote fusion.
Living with a Broad-Based Disc Bulge: Managing Your Condition
While a broad-based disc bulge can be a challenging condition, there are many steps you can take to manage your condition effectively and improve your quality of life. Following your doctor’s recommendations, maintaining a healthy lifestyle, and incorporating some preventive measures can help prevent the progression of disc degeneration and minimize future problems.
Lifestyle Modifications: Promoting Well-Being and Disc Health
- Maintain a Healthy Weight: Obesity significantly increases the stress on your spine. Losing excess weight can significantly reduce the pressure on your intervertebral discs and may help alleviate pain and improve your overall health.
- Proper Posture: Paying attention to your posture throughout the day, whether you’re standing, sitting, or lifting objects, can help protect your spine. Practice good posture by keeping your back straight, your shoulders relaxed, and your head level.
- Regular Exercise: Regular exercise can strengthen core muscles, improve flexibility, and increase blood flow to the spine, promoting healing and reducing pain. However, it is crucial to choose exercises that are appropriate for your condition and to listen to your body, avoiding activities that worsen your symptoms.
- Ergonomics: If your job or daily activities involve prolonged sitting or standing, ensure you have proper ergonomic support. Use a supportive chair, adjustable desk, and take frequent breaks to stretch and move around to prevent prolonged strain on your back.
- Stress Management: Chronic stress can contribute to muscle tension and back pain. Finding healthy ways to manage stress, such as yoga, meditation, deep breathing, or spending time in nature, can help reduce the negative impact on your back.
- Avoid Smoking: Smoking reduces blood flow to the spine and can hinder healing. Quitting smoking can improve your overall health and potentially benefit your back condition.
Seeking Help: When to Contact Your Doctor
If you are experiencing any of the symptoms associated with a broad-based disc bulge, it is essential to consult your doctor for diagnosis and treatment. While many cases can be managed with conservative therapies, early intervention can often lead to better outcomes and prevent further complications. Do not hesitate to seek professional medical advice if your symptoms are severe, persistent, or worsen over time.
Broad-Based Disc Bulge
Conclusion: A Path to Recovery and Prevention
Understanding the causes, symptoms, and treatment options for a broad-based disc bulge empowers you to navigate this common back problem effectively. By adopting healthy lifestyle habits, seeking appropriate medical care, and making informed decisions about your treatment, you can manage your condition, minimize pain, and improve your quality of life. Remember that a broad-based disc bulge doesn’t have to define you. With the right approach, you can reclaim your strength, mobility, and well-being.






